Mastiff Health
Mastiff Standard
--------------------------------------------------------------------------------
Mastiff Breed Standard
Working Group
General Appearance
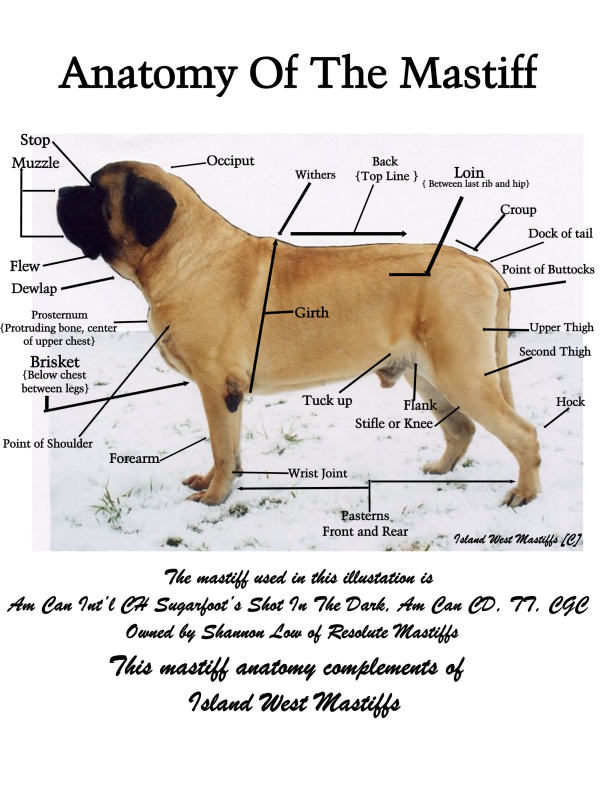
The Mastiff is a large, massive, symmetrical dog with a well-knit frame. The impression is one of grandeur and dignity. Dogs are more massive throughout. Bitches should not be faulted for being somewhat smaller in all dimensions while maintaining a proportionally powerful structure. A good evaluation considers positive qualities of type and soundness with equal weight.
Size, Proposition, Substance
Size--Dogs, minimum, 30 inches at the shoulder. Bitches, minimum, 27½ inches at the shoulder. Fault--Dogs or bitches below the minimum standard. The farther below standard, the greater the fault.
Proportion--Rectangular, the length of the dog from forechest to rump is somewhat longer than the height at the withers. The height of the dog should come from depth of body rather than from length of leg.
Substance--Massive, heavy boned, with a powerful muscle structure. Great depth and breadth desirable. Fault--Lack of substance or slab sided.
Head
In general outline giving a massive appearance when viewed from any angle. Breadth greatly desired.
Eyes set wide apart, medium in size, never too prominent. Expression alert but kindly. Color of eyes brown, the darker the better, and showing no haw. Light eyes or a predatory expression is undesirable. Ears small in proportion to the skull, V-shaped, rounded at the tips. Leather moderately thin, set widely apart at the highest points on the sides of the skull continuing the outline across the summit. They should lie close to the cheeks when in repose. Ears dark in color, the blacker the better, conforming to the color of the muzzle.
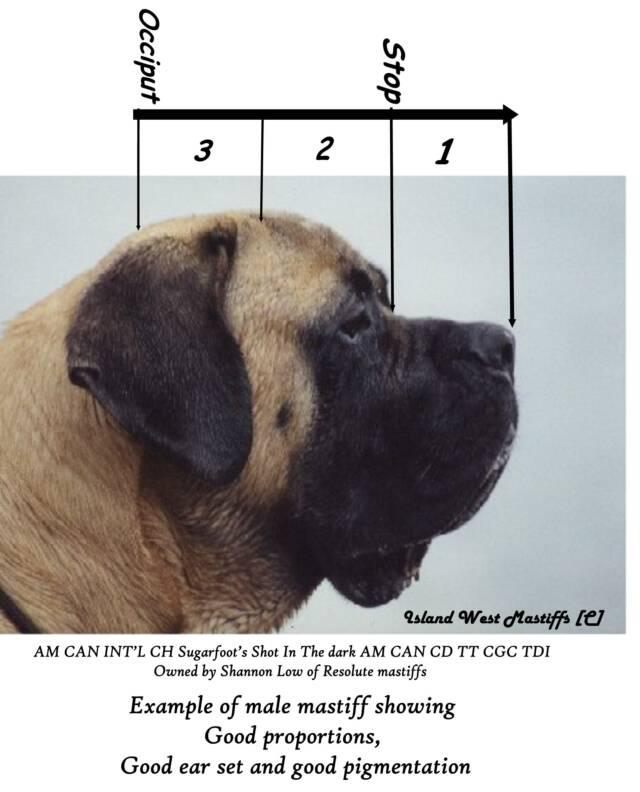
Skull broad and somewhat flattened between the ears, forehead slightly curved, showing marked wrinkles which are particularly distinctive when at attention. Brows (superciliary ridges) moderately raised. Muscles of the temples well developed, those of the cheeks extremely powerful. Arch across the skull a flattened curve with a furrow up the center of the forehead. This extends from between the eyes to halfway up the skull. The stop between the eyes well marked but not too abrupt.
Muzzle should be half the length of the skull, thus dividing the head into three parts-one for the foreface and two for the skull. In other words, the distance from the tip of the nose to stop is equal to one-half the distance between the stop and the occiput. Circumference of the muzzle (measured midway between the eyes and nose) to that of the head (measured before the ears) is as 3 is to 5. Muzzle short, broad under the eyes and running nearly equal in width to the end of the nose. Truncated, i.e. blunt and cut off square, thus forming a right angle with the upper line of the face. Of great depth from the point of the nose to the underjaw. Underjaw broad to the end and slightly rounded. Muzzle dark in color, the blacker the better. Fault snipiness of the muzzle.
Nose broad and always dark in color, the blacker the better, with spread flat nostrils (not pointed or turned up) in profile. Lips diverging at obtuse angles with the septum and sufficiently pendulous so as to show a modified square profile. Canine Teeth healthy and wide apart. Jaws powerful. Scissors bite preferred, but a moderately undershot jaw should not be faulted providing the teeth are not visible when the mouth is closed.
Neck, Topline, Body
Neck powerful, very muscular, slightly arched, and of medium length. The neck gradually increases in circumference as it approaches the shoulder. Neck moderately "dry" (not showing an excess of loose skin). Topline--In profile the topline should be straight, level, and firm, not swaybacked, roached, or dropping off sharply behind the high point of the rump. Chest wide, deep, rounded, and well let down between the forelegs, extending at least to the elbow. Forechest should be deep and well defined with the breastbone extending in front of the foremost point of the shoulders. Ribs well rounded. False ribs deep and well set back. Underline--There should be a reasonable, but not exaggerated, tuck-up. Back muscular, powerful, and straight. When viewed from the rear, there should be a slight rounding over the rump. Loins wide and muscular.
Tail set on moderately high and reaching to the hocks or a little below. Wide at the root, tapering to the end, hanging straight in repose, forming a slight curve, but never over the back when the dog is in motion.
Forequarters
Shoulders moderately sloping, powerful and muscular, with no tendency to looseness. Degree of front angulation to match correct rear angulation. Legs straight, strong and set wide apart, heavy boned. Elbows parallel to body. Pasterns strong and bent only slightly. Feet large, round, and compact with well arched toes. Black nails preferred.
Hindquarters
Hindquarters broad, wide and muscular. Second thighs well developed, leading to a strong hock joint. Stifle joint is moderately angulated matching the front. Rear legs are wide apart and parallel when viewed from the rear. When the portion of the leg below the hock is correctly "set back" and stands perpendicular to the ground, a plumb line dropped from the rearmost point of the hindquarters will pass in front of the foot. This rules out straight hocks, and since stifle angulation varies with hock angulation, it also rules out insufficiently angulated stifles. Fault--Straight stifles.
Coat
Outer coat straight, coarse, and of moderately short length. Undercoat dense, short, and close lying. Coat should not be so long as to produce "fringe" on the belly, tail, or hind legs. Fault Long or wavy coat.
Color
Fawn, apricot, or brindle. Brindle should have fawn or apricot as a background color which should be completely covered with very dark stripes. Muzzle, ears, and nose must be dark in color, the blacker the better, with similar color tone around the eye orbits and extending upward between them. A small patch of white on the chest is permitted.
Faults--Excessive white on the chest or white on any other part of the body. Mask, ears, or nose lacking dark pigment.
Gait
The gait denotes power and strength. The rear legs should have drive, while the forelegs should track smoothly with good reach. In motion, the legs move straight forward; as the dog's speed increases from a walk to a trot, the feet move in toward the center line of the body to maintain balance.
Temperament
A combination of grandeur and good nature, courage and docility. Dignity, rather than gaiety, is the Mastiff's correct demeanor. Judges should not condone shyness or viciousness. Conversely, judges should also beware of putting a premium on showiness.
Approved November 12, 1991
Effective December 31, 1991
Spaying or Neutering your Mastiff
Most veterinarians recommend spaying or neutering a puppy at or before six months of age. With animal shelters full of accidentally bred dogs and their puppies, their belief in early altering is understandable. Vets also recommend to spay early to prevent mamary (breast) cancer in females and neuter to avoid temperament or marking issues or testicular cancer in an intact male. Most veterinarians, however, have little first-hand knowledge about Mastiffs and the special needs associated with these big guys. Early spaying/neutering is NOT recommended for giant breed dogs. Mastiffs need the hormones present when they reach sexual maturity to reach their full potential physically. Spaying and neutering early (before at least a year old) often has adverse effects on both the look and health of a Mastiff. A Mastiff's growth plates need the hormones to close, as well as to develop bone density.
Females: Mamary cancer is a rarity, and chances of contracting it or other reproductive system cancers goes up only slightly when spaying at over a year of age versus spaying at under a year old, but it's been proven that spaying early does increase the chance of her contracting bone or lung cancer later in life or developing permanent problems with incontinence and bladder leakage that are often tough to deal with. Mastiffs need the hormones of at least the first heat cycle to help their organs mature and develop. Anyone who owns a female Mastiff can tell you how much their girl "bloomed" after her first heat cycle. Also, puppies that are prone to frequent urinary tract infections (UTIs) often outgrow them after their first heat cycle. Mastiffs usually come into their first heat at about 9-12 months of age. An average heats last 3 weeks, which is a minor inconvience that makes a world of difference in your girl's overall health. Just be sure to take precaustions so she is not accidentally bred, either by your own male or a neighborhood dog. Some people opt to board their girls while they're in heat to make sure this doesn't happen.
Males: The chance of a male Mastiff developing cancer later in life from being neutered closer to 2 years of age instead of earlier is very slight. However, when male Mastiffs are neutered too young, before their hormones are at full tilt, they often do not gain the muscle or mass that an adult male should have and tend to look like a gangly puppy their whole life. Neutering males early usually effects overall bone size, and you end up with a tall, lanky dog with no bone and a small head--they end up looking like badly bred Great Dane, not a Mastiff. Mastiffs need their sexual hormones for proper growth. If you buy a well-bred Mastiff, you want one that looks like a Mastiff, not a Dane.
If you spay or neuter after a year and before two years of age, you still get many of the same health benefits for your dog that comes with an early spay or neuter, without the negatives. We recommend spaying and neutering around 18 months of age. Remember, Mastiffs are not just big Labs. They are a special breed with needs all their own. Small breeds often do well when spayed or neutered at an early age, but with giant breeds it is better to wait. **NOTE If your dog will be sedated for any surgery or procedure, be sure to tell your veterinarian "NO ACE." Acepromazine is a commonly used tranquilizer for dogs and cats, and has been known to slow the heart down so much in our guys that they never wake up, dying on the table or shortly after. Always remind your vet's office.
In keeping with the spirit of the MCONO Code of Ethics, Mastiff breeders are encouraged to inform puppy buyers of developmental conditions (that may or may not be hereditary or genetic) that are known to exist in Mastiffs, as well as methods to test and/or monitor some of these conditions.
Please keep in mind that all purebred and mixed breed dogs can have health concerns and health testing is simply a tool....not a guarantee.
EYE PROBLEMS IN THE BREED
• Canine Multi-focal Retinopathy (CMR), also known as Retinal Dysplasia/Retinopathy - Abnormal development of the retina present at birth and recognized to have three forms: folds, geographic, and detachment. A Mastiff with folds will currently pass CERF and the folds may disappear over time while the geographic and detached forms may cause loss of vision or blindness. There is a DNA test available though OptiGen www.optigen.com for CMR in Mastiffs.
• Cataract - Lens opacity that may affect one or both eyes and some forms may cause blindness.
• Distichiasis - Eyelashes abnormally located in the eyelid margin which may cause ocular irritation.
• Ectropion - Conformational eyelid defect, which may cause ocular irritation due to exposure.
• Entropion - Conformational defect where eyelid margins invert or roll inward, toward the eye causing eyelashes and hair to rub against the cornea which may result in ocular irritation.
• Macroblepharon - Abnormally large eyelid opening; may lead to secondary conditions associated with corneal exposure.
• Persistent Pupillary Membranes (PPM) - Persistent blood vessel remnants in the anterior chamber of the eye which fail to regress normally in the neonatal period.
• Progressive Retinal Atrophy (PRA) - Degenerative disease of the retinal visual cells which leads to blindness. In Mastiffs the age at which PRA can be detected varies from as young as 6 months to as late as 42 months. Typically Mastiffs with PRA go blind gradually, first loosing their night vision and then their day vision. Many do not go completely blind until they are 8 years old or older. There is a DNA test available through OptiGen www.optigen.com for PRA in Mastiffs.
ORTHOPEDIC, NEUROLOGICAL, STRUCTURAL, AND JOINT PROBLEMS IN THE BREED
• Anterior Cruciate Ligament (ACL) Rupture - The knee along with the external support (i.e., collateral leg) has two ligaments inside the joint that help prevent forward movement (i.e., cruciate). Insult/injury can cause this ligament to rupture and result in acute lameness (not want to bear weight) on the limb.
• Degenerative Myelopathy (DM) – This is a progressive, degenerative, late onset disease of the spinal cord seen in older dogs. The symptoms usually begin with hind end weakness, lack of coordination and shuffling or dragging of the rear feet. There is a DNA test for DM through OFA www.offa.org
• Elbow Dysplasia - Elbow dysplasia encompasses several different conditions, all of which are indicative of abnormally formed or fused elbow joints and all can cause lameness and pain:
o Fragmented Coronoid Process (FCP) - This form of elbow dysplasia is generally the most difficult to treat if the fragments are actually loose in the joint.
o Osteochrondritis Dissecans (OCD) - A defect in the joint cartilage overlaying or attaching to the bone. OCD most commonly occurs in the elbows, shoulders, hocks and stifles.
o Ununited Anconeal Process (UAP) - In giant breeds such as Mastiffs the Anconeal Process can close later than in smaller breeds, often as late as one year of age or older.
• Hip Dysplasia - Hip dysplasia is a painful condition caused by abnormally formed hips. The animal may become lame in the hind quarters due to the pain associated with the degeneration of the hips.
• Hypertrophic Osteodystrophy (HOD) - A developmental disorder that manifests with toes turning in or out, roached toplines, pinched rears, and in advanced stages fever, lethargy, pain in joints, inability to stand or function. This is a problem of intake in calories versus output of energy - too many calories consumed and/or unbalanced diet disrupted by supplementing.
• Panosteitis (Pano or Wandering Lameness) – A developmental problem that affects the long bones during rapid growth periods typically between 6-16 months of age. The exact cause is unknown although genetics, diet, stress, infection, and metabolic or autoimmune problems have been suspected. Lameness can occur in one limb or over time in all limbs. It often is intermittent affecting one leg then another and back again… It is self-limiting and spontaneously disappears.
• Spondylosis – is a degenerative disease that causes excessive bone production of osteophytes along the spinal vertebrae which can cause lameness. In advanced cases the vertebrae can fuse together. In many cases there are no clinical symptoms, but the acute expression of the disease such as lameness, severe pain and disabilities are often seen in adults and older Mastiffs.
• Wobblers Syndrome – Cervical Vertebral Instability (CVI) is caused by pressure and pinching of the cervical spinal cord and the nerves in the neck due to ligament problems and/or vertebrae malformation. The compression on the spinal cord in the neck may cause the Mastiff to stand and move abnormally. This is believed to be an inherited genetic disorder with environmental influence. Rapid growth and nutrition may influence the expression of the disease.
MISCELLANEOUS OTHER PROBLEMS IN THE BREED
• Allergies – Some Mastiffs have allergies to certain foods, pollens, etc. Allergies are due to autoimmune problems and since they often run in certain lines they are believed to be inherited.
• Cancer - Most forms of cancer have been diagnosed in some members of the breed. Cancer can be hereditary while others occur spontaneously or even due to environmental toxins. Although there are several forms of cancer found in Mastiffs, the most common types are: Osteosarcoma (Bone Cancer), Lymphoma, Hemangiosarcoma, Mast Cell Tumors, Squamous Cell Tumors, & Breast Cancer. Today there are advanced medical treatment options such as radiation, chemotherapy and medications to reduce the size of the tumors and offer pain management to help maintain a good quality of life.
• Cystinuria - An inherited metabolic disease caused by a defective kidney transporter for cystine and some other amino acids. Because cystine readily precipitates in acid urine, crystals and later calculi (stones) can form in the kidney and bladder. Cystinuria in Mastiffs primarily affects males and can result in serious illness and may be life threatening.
• Epilepsy – A seizure disorder which can have multiple causes. The age of onset of the inherited form is normally around 6 months to 5 years of age. Epilepsy is often difficult to treat successfully in Mastiffs and other large breeds.
• Gastric Dilation, Torsion, Volvulus (Bloat) - Bloat is a hideous killer of giant breed animals, and Mastiffs are no exception. Without warning, the stomach fills with air (dilation), can twist 180 degrees (torsion) on its long axis, or more than 180 degrees (volvulus) thereby cutting off blood and oxygen to vital organs. Bloat can be primary or secondary, caused by emotional or physical stress, improper nutrition or feeding habits, guzzling water, inappropriate exercise, as well as other causes that we do not understand. Every Mastiff owner needs to familiarize themselves with bloat symptoms and have a plan of action to get the animal to an emergency medical facility at the onset of the first symptom. A dog that is bloating often has approximately 3 hours to live without medical intervention.
• Heart Disease - The most common heart problems in Mastiffs are aortic stenosis, mitral valve dysplasia and cardiomyopathy. Early detection and treatment are essential for a good prognosis. Some mastiffs have heart murmurs that are mild and not a cause for concern. If a heart murmur is detected it is essential to have it checked to see if it is an "innocent" murmur or a serious problem.
• Hypothyroidism - Hypothyroidism is the result of an abnormally functioning thyroid gland resulting in a lower than normal level of thyroid hormone. This lack of thyroid hormone can have serious health consequences including coat and skin problems, intolerance to cold, weight gain or loss, infertility, sudden aggression, and immune system malfunctions. The inherited form is autoimmune thyroiditis where the body's own immune system attacks and destroys the thyroid gland or reduces its function. Autoimmune thyroiditis is diagnosed by measuring the FT4D, cTSH & TgAA. Acquired hypothyroidism can be caused by various problems such as stress for long periods of time, poor nutrition, prolonged infections, and chemical agents.
• Reproductive Issues – There are several reproductive problems that can affect Mastiffs and it is encouraged that you research this area if you plan to breed. Some of the most common are pyometria (uterine infection), cryptorchidism (undescended testicles), failure to conceive, and vaginal hyperplasia.
• von Willebrand's Disease (vWD) - A rare abnormal bleeding disorder due to a lack of normal clotting. An animal's life can be threatened by bleeding due to an injury, or during spaying/neutering or any other condition resulting in bleeding.